Many people live for years with ongoing digestive symptoms – pain, bloating, diarrhea, constipation, nausea, reflux, or unpredictable bowel habits – without a clear explanation. When tests come back “normal,” it can feel confusing and discouraging, especially when symptoms are persistent and disruptive.
It’s very common to worry that something has been missed, and many people feel caught between two realities: the symptoms feel severe, but investigations don’t show a clear cause.
In many cases, ongoing symptoms like these are linked to what's called a disorder of gut-brain interaction (DGBI).
This guide provides a clear explanation of the gut-brain mechanisms that can drive persistent symptoms – and how DGBIs are manageable with the right approach.
What is a disorder of gut-brain interaction?
Your gut and your brain are more connected than most people realize.
They constantly ‘talk’ to each other through nerves, hormones, immune signals, and chemical messengers that help regulate digestion and interpret gut sensations.
One of the main pathways is the vagus nerve, which acts like a communication super highway between the digestive system and the brain.
A disorder of gut-brain interaction (DGBI) is when this communication system becomes disrupted or hypersensitive.
With DGBIs, symptoms aren’t caused by visible damage or disease in the digestive tract. Instead, they’re driven by changes in how gut signals are sent, amplified, and interpreted by the nervous system.
Types of gut-brain disorders
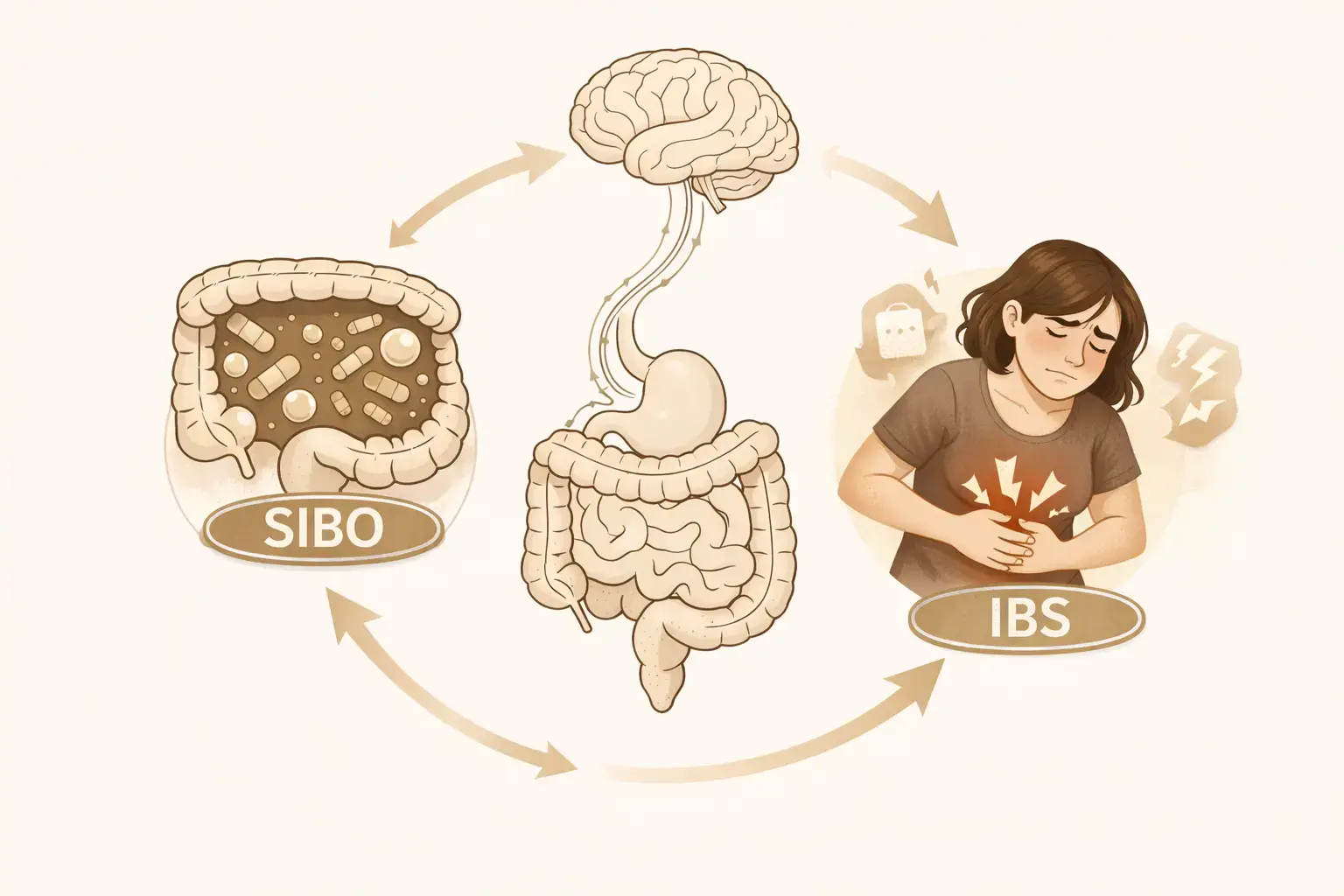
Common digestive disorders with a gut-brain link include:
- irritable bowel syndrome (IBS)
- functional dyspepsia
- reflux hypersensitivity
- functional constipation
- functional diarrhea
- other functional bowel disorders
These conditions can look different on the surface, but they share a common underlying feature – altered gut-brain communication.
They are also extremely common, affecting millions of people worldwide.
So, if you’ve been diagnosed with one of these conditions, you are not alone – and your symptoms fit a well-recognized medical pattern.
How gut-brain signaling creates symptoms
Think of the gut-brain connection like a volume dial.
Everyone has a built-in system that controls how strongly sensations from the gut are felt. Most of the time, that dial is set low – digestion happens quietly in the background, and you barely notice it.
In some people, the sensory nerves in and around the gut become more sensitive. This means everyday digestive activity – such as movement, gas, fullness, or bowel contractions – can feel louder or more intense than usual, even though the gut itself isn’t damaged.
This increased reactivity of the gut’s nerves is known as visceral hypersensitivity.
When these stronger signals reach the brain, the brain may interpret them as a problem – even when nothing harmful is happening. In response, it can send stronger signals back to the gut, which can further amplify symptoms such as:
- discomfort or pain
- urgency
- bowel changes
- bloating or distension
- nausea or reflux symptoms
Once this volume is turned up, the pattern is reinforced and symptoms can be triggered more easily – even by normal digestive processes.
Brain-gut therapy, tailored to you
Fix the miscommunication between your back and brain
Overcome life's challenges
Take control of hot flashes and night sweats
Quit smoking in 3 weeks
Why answers can feel hard to find: Understanding 'normal' results
Many people assume that persistent, painful symptoms must come from visible disease. It’s a reasonable assumption – and why healthcare providers take symptoms seriously and often order tests.
The reason for this is that not all medically significant conditions show up clearly on imaging, scopes, or blood work. Gut-brain disorders are diagnosed based on symptom patterns and physiology, not structural damage.
Therefore, a normal test result does not mean nothing is happening.
It just means there is no evidence of a dangerous structural condition such as inflammatory bowel disease, ulcers, or cancer.
Once structural diseases have been ruled out, the focus often shifts toward understanding the type of gut-brain dysfunction that may be driving your symptoms.
But for many people, that shift can feel difficult at first – especially if symptoms continue, change, or flare unpredictably.
In that situation, it is completely understandable to want more testing. A normal scan or blood test can bring temporary relief, but that reassurance often fades when symptoms return. Over time, this can create a cycle where ongoing symptoms lead to repeated investigations, and repeated investigations reinforce the feeling that there must be a hidden cause that still hasn’t been found.
This does not mean further testing is never appropriate. It simply means that once structural disease has been ruled out, the most helpful next question often becomes: “What is driving this symptom pattern, and why is the gut-brain system staying on high alert?”
Why gut-brain explanations are not dismissive
If tests have ruled out disease, it can still be hard to hear terms like ‘hypersensitivity’, ‘nervous system’, or ‘stress response’, because many people worry it means their healthcare provider believes the symptoms are psychological.
But when it comes to DGBIs, it’s critical you understand it’s never ‘all in your head’. And a gut-brain explanation is a physiological explanation.
It describes how the nervous system interacts with the digestive tract and how symptoms can be amplified. It also explains why symptoms can be intense and disruptive even when no structural disease is present.
Why your symptoms can feel unpredictable
If you have a gut-brain disorder, it’s likely you’ve noticed your symptoms fluctuating: some days may feel manageable, while others feel overwhelming. This unpredictability can be difficult to understand and hard to plan around.
Because the gut-brain system is responsive, symptoms can be influenced by many factors, including:
- digestion itself
- sleep disruption
- prior flare-ups
- hormonal changes
- illness or antibiotics
- heightened nervous system alertness
In many cases, symptoms are not tied to a single trigger. Instead, they reflect a system that has become more reactive over time.
Can DGBIs be fixed by diet?
Many people with a gut-brain disorder assume their symptoms must be caused by something they ate, especially if flare-ups seem connected to meals. While food can certainly act as a trigger for symptoms, it is not usually the underlying cause of a gut-brain disorder.
Foods – including those high in FODMAPs – naturally create pressure, gas, and movement in the digestive tract. This happens to everyone.
The difference is that in people with a gut-brain disorder, the nerves in the gut are more sensitive and the system is more reactive overall.
Because of this heightened sensitivity, normal digestive processes can be felt more strongly and interpreted by the brain as discomfort or pain, even when nothing harmful is happening. This means everyday foods may sometimes lead to outsized symptoms, not because the food itself is damaging, but because it is passing through a sensitized system.
Dietary changes and medications can help reduce symptoms for some people by lowering digestive load or calming reactivity. However, they do not retrain the gut-brain signaling system itself.
This is one reason symptoms can return, shift, or flare unpredictably over time – even when someone is doing ‘all the right things’.
You are not imagining this
Gut-brain disorders are real, medically recognized conditions.
If you have felt dismissed, confused, or unsure whether your symptoms ‘count’, this is important to know: there is a clear medical explanation for what you are experiencing.
Understanding the gut-brain mechanism can reduce uncertainty and help you feel more confident as you continue care with your healthcare provider.


.webp)






