It may seem daunting and feel like your favorite foods are off the menu forever, but here are the steps you can take to move forward, rethink restrictive behaviors, and enjoy eating again.
Why restrictive diets are not the solution
Following a restrictive diet can affect your relationship with food and your mental well-being—it’s hard telling yourself ‘No!’ all the time. And a challenging elimination diet like the low FODMAP diet was never designed as a long-term solution, nor is it a quick DIY fix. Instead, it’s a short two- to six-week process best followed under the guidance of a healthcare practitioner who leads you through the diet’s three key phases (elimination, reintroduction, and personalization).
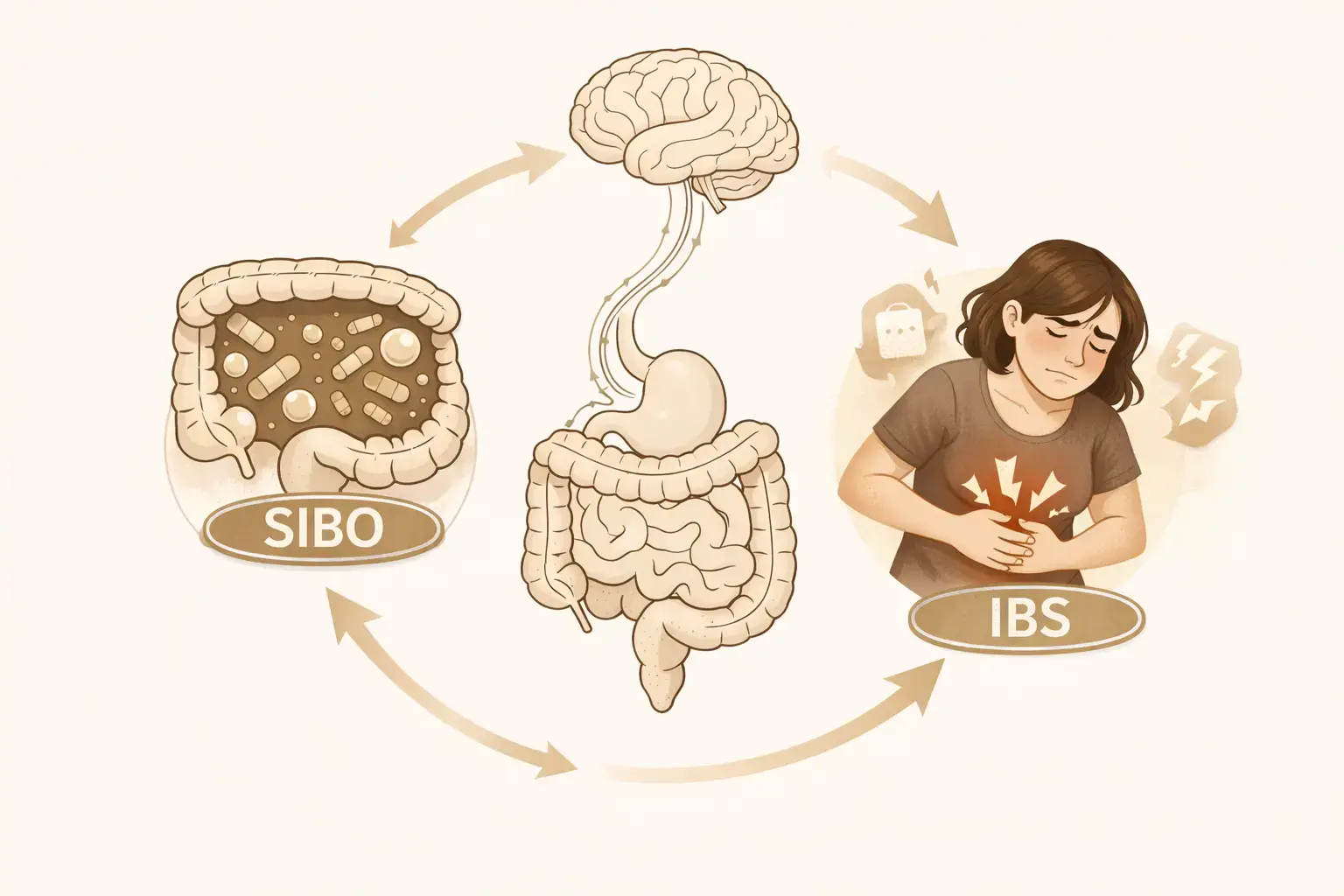
Research shows that people who try following restrictive diets in the long term are more likely to engage in disordered eating behaviors, including binge eating, restricting, and compensatory behaviors. Being on a restrictive diet for extended periods can also reduce the diversity of bacteria in your gut microbiome, which can impact your mental health too—95% of serotonin, the happy hormone, is produced by your gut microbiome.
It’s also common for people to experience the ‘forbidden fruit’ phenomenon, which is when not being able to have something makes you want it even more. When you eventually cave and allow yourself to have some, the ‘What the heck?’ effect appears. This is when you think to yourself, ‘Oh well, I’m off track now, I might as well finish it off and go back for seconds’, which is not the best way to manage symptoms in the long term.
How to create a flexible relationship with food
Flexibility is the key to developing long-term healthy habits, even if you are managing food intolerances. Here’s how you can move away from restrictive eating (and thinking) and start embracing a more flexible approach.
1. Talk it through
Think about what you want overall, not just what your taste buds want. While a mouthful of food you’ve been craving can feel wonderfully indulgent, sometimes our taste buds want the opposite of what our stomach needs.
Before you eat something you’re unsure about, take a quick time-out to consider asking yourself first, ‘How do I want to feel after eating?’ or ‘Which foods will satisfy the sensations I get during and after eating?’ Talking it through in your mind first will help you focus on whether a particular food will lead to a positive outcome.
2. Know what works for you
Get to know the foods you enjoy and your gut tolerates, and give yourself permission to eat them freely. Mentally allow yourself to choose how much and how often you want to eat them.
When practicing this mindfully, you might naturally choose to eat the amount that suits you best (which may be none). The key difference is that you are giving yourself permission to make the choice, rather than being dictated by food rules and pre-determined portion sizes. Just keep in mind, if you have allergies, this may not apply. It’s best to chat with a healthcare clinician about your individual circumstances.
3. Discover your options
There are so many new habits and ways of thinking to explore that will help you move away from restrictive eating patterns and towards a more peaceful approach to mealtimes. The best way to know your options is to reach out to a dietitian or healthcare professional for tailored advice. Not everyone enjoys the same foods, and gut symptoms can vary widely.
Learning how to eat mindfully while still keeping your specific intolerances or allergies in check will help you move away from restrictive thinking habits.
Letting go
It can be upsetting when you’re craving a particular food and your gut isn’t having it. Choosing not to eat foods that irritate your symptoms can come with feelings of sadness, frustration, anger, disappointment, or disconnection. But finding ways to practice compassion, self-soothing, healthy distraction, and acceptance can be helpful for letting go of difficult emotions.
Here’s how you can put this into practice.
1. Practice self-compassion
Self-compassion and refocusing your thoughts can significantly impact your relationship with food. To shift the way you think and talk to yourself, try practicing cognitive defusion techniques, which are like an internal circuit breaker for your mind. They will help shift your focus away from restrictive eating and negative self-talk, and help you move towards a more positive approach to food and the way you think about your own habits.
If you tend to be your harshest critic, one cognitive defusion technique is to imagine you’re speaking to a friend. Picture you telling them to let go of certain foods and concentrate on what they can eat and enjoy. By not speaking so harshly and directly to yourself, the thoughts become less ‘fused’, helping you gain a new perspective.
2. Soothe yourself
Practice self-soothing to help you feel calm and relaxed—just not eating for comfort. Try listening to gut-directed hypnotherapy and learning diaphragmatic breathing, collating a playlist of your favorite songs so it’s always on hand, exercising, or scheduling time with friends. Whatever you like and enjoy will help you manage the big emotions you may be feeling with your diet.
3. Divert your attention
Rather than getting caught up in thoughts about the foods that you’re missing out on, try to pay attention to the benefits of choosing foods that give you longer-lasting pleasure, energy, fulfillment, and are the least likely to bring on unwanted symptoms.
4. Accept what is out of your control
While hearing you need to ‘just accept’ your food intolerances can be infuriating, ultimately, you are better off accepting things you can’t change and moving on, rather than getting caught up in fighting the reality of having IBS and gut health issues.
Reframing how you ‘just accept it’ might help you see your gut health and symptoms in a new way. You could try rewording it to:
- drop the struggle
- let it be
- breathe into it
- give it some space
- stop fighting it
- make room for it
- it is what it is.
Give yourself some space to notice the feelings that arise and acknowledge that, yes, IBS and food intolerance can be hard to ‘just accept’.
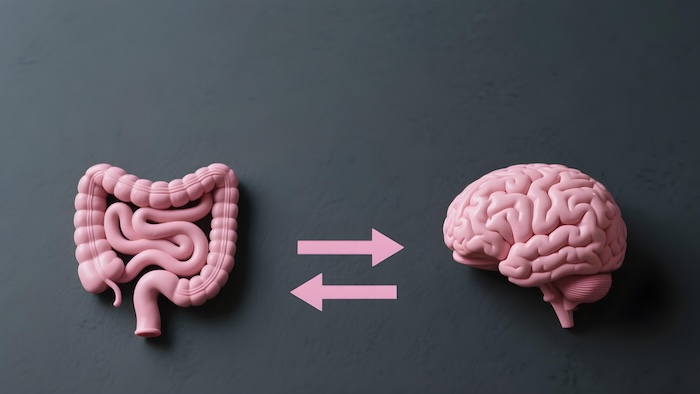
Brain-gut therapy, tailored to you
Fix the miscommunication between your back and brain
Overcome life's challenges
Take control of hot flashes and night sweats
Quit smoking in 3 weeks
Be prepared
You can’t eat food you don’t have access to, right?
You’re much more likely to order takeout or eat something your gut won’t be happy about if your kitchen isn’t stocked with the right foods.
Take a few minutes to consider your habits for meal planning, budgeting, shopping lists, regular grocery shopping, bulk prepping, using leftovers, and so on. You need to make it as easy as possible to feel organized and on top of your food and eating behaviors. Reaching out to a dietitian or nutritionist can help you better understand what to eat, but also how to rethink your eating and cooking habits as a whole.
Navigating comments from others
While you might know your triggers and have a good grasp of your intolerances, this won’t stop well-meaning friends and family from pushing you to go against your better judgment, telling you, “Oh go on, just a little bit won’t hurt.”
While it can feel like you’re being pressured to eat foods you’re not comfortable with, it’s likely they have good intentions, such as they want to be a good host if you’re sharing a meal in their home or they don’t want you to feel like you’re missing out.
Instead of lashing out or caving in and eating foods you’d rather not, try these responses the next time you’re feeling pressured and uncomfortable:
- “I really appreciate that you care, you’re so generous, but if I eat that I’ll feel uncomfortable later and I don’t think you want me to feel unwell.”
- “Thank you, I’d honestly love to taste it, but I’m finding that I’m feeling better without eating [this food] at the moment, thank you.”
- “You’re so kind to share, but I’m happy to help myself if I want some later.”
On the other hand, if you’ve been vocal about not eating a certain food but you’ve moved through an elimination diet and are in the stage of reintroducing foods and finding you can tolerate different things, it’s OK to change your mind! You can tell friends and family that you are choosing to eat a formerly restricted food as you’ve been working through your intolerances, sharing as much or as little information as you’re comfortable with.
Adapting to changes
Remember that an intolerance to a FODMAP is not an allergy, but it’s not a deadly disease either. Some bloating and fluctuations in your bowel habits are very normal, and aiming for perfection is unrealistic and often counterproductive.
The majority of people with IBS find they can tolerate a certain amount of high FODMAP foods. However, what that ‘certain amount’ is can vary widely, and it’s best identified through the reintroduction process, which is phase two of the low FODMAP diet.
The other consideration is your tolerance threshold can change over time. It may be worth revisiting the reintroduction process with a dietitian to explore your current tolerances as you may be restricting foods unnecessarily.
Mindful and intuitive eating
Mindful eating and intuitive eating principles encourage us to pay attention with curiosity, and increase our awareness of the eating experience and the body’s physical sensations.
To start, practice pausing before eating, reduce or remove distractions, and pay attention to the look, smell, taste, and texture of food. Then, be curious about how the food feels in your body and learn from each eating experience.
There will be times when perhaps you’re dining out with friends and food envy strikes. You’ll see your friend eating something that looks really appealing, but you’ll tell yourself, ‘That’s off limits for me and I’ll probably feel sick if I try some.’
Getting caught in this mentality can prevent you from experiencing pleasure we get from other senses, like sight, smell, touch, and sound. Try tuning into other sensations you feel in your body: how does the food smell? Is that a pleasant sensation? How does it look?
The Wrap Up
It can be daunting to think you might never get to enjoy your favorite foods again if you know you have dietary intolerances. But there are steps you can take to rethink your restrictive habits and start creating a long-term plan. You can learn how to create a more flexible relationship with food, practice self-compassion to start letting go of what your gut just won’t tolerate, get a food prep system in place to help you side step flare-ups, learn to navigate difficult food-based conversations, and try mindful, intuitive eating.
About Molly Warner, APD
Molly Warner is an Accredited Practicing Dietitian, Certified Intuitive Eating Counsellor, and Credential Eating Disorder Clinician. She helps people who struggle with gut health and dieting issues to navigate food intolerances and heal their relationship with food so they can feel calm inside, confident with food choices and ultimately, satisfied. Living with Coeliac Disease, she gets what it’s like to live with dietary restrictions. She’s been there; wanting some help getting into a rhythm of eating that helps the body to function at its best. She is here to guide and empower you to live and eat in a way that frees you from gut symptoms and ‘diet culture’ and truly nourishes your wellbeing.
Contact Molly for IBS management support and guidance

.avif)
.webp)