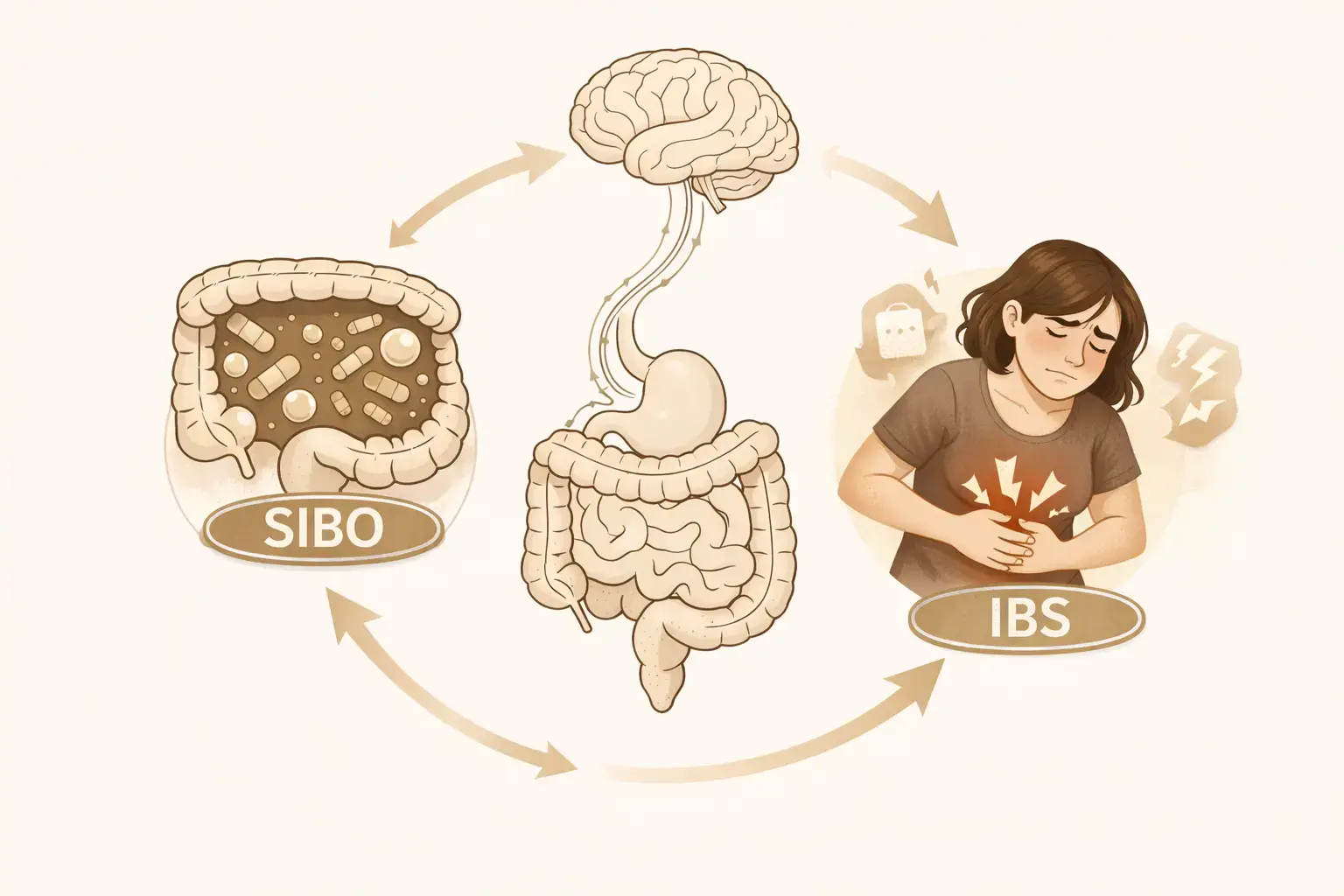
SIBO vs IBS: What’s the Connection?
If you’ve been dealing with bloating, abdominal pain, diarrhea, constipation, or unpredictable flare-ups, you may have come across two common explanations: SIBO and IBS.
They can look almost identical. But they aren’t the same condition.
SIBO is a pattern of bacterial overgrowth in the small intestine.
IBS is a disorder of gut-brain interaction, where the nervous system plays a major role in how gut sensations are processed. [1]
For some people, SIBO may contribute to IBS-like symptoms. For many others, IBS symptoms continue even when SIBO is treated.
Understanding the difference can help you avoid getting stuck in testing and treatment loops that don’t lead to lasting relief.
What Is SIBO?
SIBO stands for small intestinal bacterial overgrowth.
Normally, the small intestine contains relatively low levels of bacteria compared with the colon. In SIBO, bacteria build up in the small intestine, where they begin fermenting food too early in digestion.
This can lead to symptoms such as:
- Bloating and visible swelling of the abdomen
- Excess gas
- Abdominal discomfort
- Diarrhea or constipation
- Symptoms that worsen after eating
SIBO often happens because something is interfering with the gut’s normal “self-cleaning” movement, rather than because bacteria are the only problem. [2]
What Is IBS?
IBS (irritable bowel syndrome) is one of the most common digestive disorders.
It’s defined by:
- Recurrent abdominal pain
- Changes in bowel habits (diarrhea, constipation, or both)
- Bloating and discomfort
IBS is now classified as a disorder of gut-brain interaction, meaning symptoms are strongly shaped by communication between the gut and the nervous system. [1]
IBS is linked to things like:
- An extra-sensitive gut (normal stretching can feel painful)
- Changes in how quickly the intestines move
- Stress-response signals affecting digestion
- Changes in microbiome and immune signaling
- The brain “turning up the volume” on gut sensations
That’s why IBS symptoms are very real, even when tests like scans or bloodwork look normal.
How Are SIBO and IBS Related?
Some People With IBS Test Positive for SIBO
Some research suggests that a subset of people diagnosed with IBS have evidence of bacterial overgrowth on breath testing. [2]
In those cases, treating suspected overgrowth may improve symptoms.
But estimates vary widely depending on how SIBO is tested and defined, which is why experts caution against assuming SIBO is the main cause of IBS for everyone.
Slow Gut Movement May Link the Two
One of the clearest connections is motility, which simply means how well the intestines move food and bacteria forward.
The small intestine normally has regular waves of movement that help sweep bacteria along. If this movement slows down, bacteria have more time to build up in the wrong place. [2]
This can be especially relevant after a stomach infection, when gut function and gut-brain signaling may stay disrupted. [1]
Can SIBO Trigger IBS Symptoms?
Yes, and this is one of the most helpful ways to think about it.
A practical model is:
- SIBO can increase gas and bloating
- IBS can make the gut more sensitive to that bloating
- The gut-brain axis determines whether bloating becomes pain, urgency, or distress
Many people with IBS have what researchers call visceral hypersensitivity, meaning the gut becomes extra sensitive to normal stretching or pressure. [1]
So SIBO may add more gas and distension, while IBS affects how strongly the body reacts to it.
This also helps explain why symptoms sometimes persist after antibiotics: reducing bacteria doesn’t automatically reset the nervous system’s sensitivity.
How Is SIBO Diagnosed?
Breath Tests Are Common, but Not Perfect
Most people are diagnosed with SIBO using hydrogen or methane breath tests.
These tests measure gases produced by bacteria after drinking a sugar solution.
Breath tests can sometimes be useful, but major experts highlight serious limitations:
- Lactulose tests may reflect how fast food moves through the gut rather than true overgrowth
- False positives and false negatives are common
- Results don’t always match symptom severity
- Testing methods and cutoffs vary widely
The Mayo Clinic has published a detailed critique warning against overreliance on breath testing, especially in IBS populations. [3]
A positive test does not automatically mean SIBO is the main cause of symptoms.
Small Intestine Sampling Is More Direct, but Rare
The most direct test involves collecting fluid from the small intestine during an endoscopy, but this is invasive and not commonly used outside research settings.
Evidence-Based Treatments for SIBO
Treatment depends heavily on the underlying cause.
Antibiotics
Rifaximin is commonly used and has evidence of benefit in some patients, especially those with diarrhea-predominant IBS symptoms. [4]
However, symptoms often return if the underlying drivers (like slow motility) are not addressed.
Diet Changes
Reducing fermentable carbohydrates (such as through a low FODMAP diet) can help reduce bloating and IBS symptoms. [5]
Diet is often most helpful as a symptom-management tool, not a permanent solution.
Supporting Gut Movement
Because slow gut movement is a major contributor to bacterial buildup, preventing relapse often requires addressing motility, not just bacteria. [2]
This is one reason repeated antibiotic cycles alone often fall short.
Where Brain-gut Therapy Fits In
Many people get stuck in cycles of:
- Ongoing symptoms despite treatment
- Fear of eating or flare-ups
- Constant attention to gut sensations
- A stress response that keeps the gut “on high alert”
Because IBS is fundamentally a gut-brain interaction disorder, treatments that target the brain-gut axis have strong evidence.
Systematic reviews show it can significantly improve IBS symptoms, with long-lasting benefits comparable to many medical therapies. [6]
The British Society of Gastroenterology guidelines recommend brain-gut therapies as part of evidence-based IBS care. [5]
For people with overlapping IBS and suspected SIBO, this matters because:
- SIBO may contribute to bloating
- IBS drives symptom sensitivity
- Gut-brain therapy helps reduce the nervous system’s overreaction
An integrated approach often works better than chasing bacterial eradication alone.
When to Talk to a Doctor
You should speak with a gastroenterologist if you have:
- Unexplained weight loss
- Blood in stool
- Persistent vomiting
- Anemia
- Symptoms that wake you from sleep
- Rapidly worsening symptoms
These are not typical IBS features and require further evaluation.
The Bottom Line
SIBO and IBS overlap, but they are not the same condition.
- SIBO can contribute to bloating and fermentation in some people
- IBS is a broader gut-brain sensitivity disorder
- Breath tests are imperfect and should be interpreted cautiously
- Treatment works best when addressing both gut physiology and nervous system sensitivity
For many people, lasting improvement comes from combining medical care with evidence-based gut-brain therapy.

.webp)







