IBS and anxiety often go hand in hand – learn how the brain-gut connection drives symptoms and what you can do to start feeling calmer and more in control.
IBS and anxiety symptoms
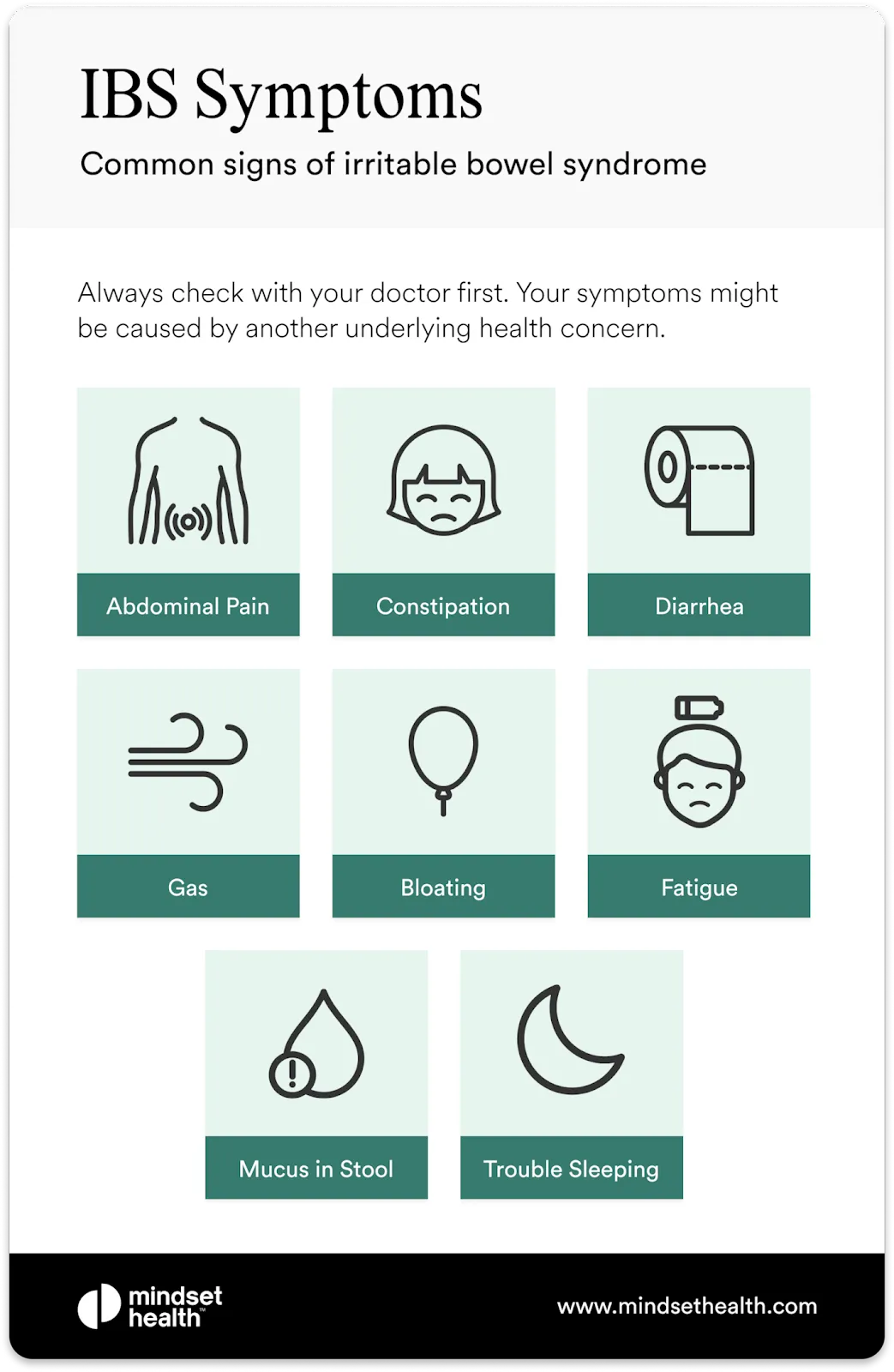
IBS and anxiety can impact everyone differently. While this can lead to different treatment options and interventions, these are the most common symptoms.
IBS symptoms
- bloating
- gas
- abdominal pain
- constipation
- diarrhea
- changes in your stool
- feeling an urge to move your bowels but are unable to do so
- incomplete bowel movements
- feeling an urgent need to move your bowels.
Anxiety disorder symptoms
- feelings of unease
- shortness of breath
- restlessness
- panic and fear
- nausea.
Connecting IBS to anxiety
IBS and mental health issues, such as anxiety and depression, commonly occur together. And studies have found that the higher your anxiety, the worse your IBS symptoms.
Often anxious feelings arise from your gastrointestinal (GI) tract and worrying that a flare-up is always just around the corner.
However, anxiety doesn’t cause IBS, and IBS doesn’t cause anxiety. However, the two disorders are known to exacerbate each other, leading to what’s often described as gastrointestinal-specific anxiety (GSA).
What causes IBS?
While there’s no known cause of IBS, several scientific theories have been put forward to explain its origins.
Traumatic life events, food allergies, and various illnesses have all been thought to play a role in why someone might develop IBS symptoms.
Other additional factors that may be contributing to ongoing persistent IBS include:
- altered pain perception
- increased gut sensitivity
- acute or chronic stress
- problems with your immune system.
While nailing down precisely what is causing your IBS isn’t possible and it can’t be prevented, it’s important to keep in mind it’s a condition that can be managed.
Brain-gut therapy, tailored to you
Fix the miscommunication between your back and brain
Overcome life's challenges
Take control of hot flashes and night sweats
Quit smoking in 3 weeks
Why IBS worsens anxiety
Researchers have shown that IBS can take a devastating toll on a person’s psychological state. For some, it can even lead to suicidal ideation.
One of the simplest ways of understanding how IBS increases anxiety is by thinking about what happens when you experience symptoms.
Cramping, bloating, pain, diarrhea, and constipation can all be incredibly distressing to endure. This can lead you down further thought spirals, telling yourself it will never end. And so many people with IBS ruminate endlessly on flare-up fears, which only leads to more mental distress and these stress levels can worsen anxiety disorders.
Social stress can also significantly contribute to chronic anxiety for people with IBS. Often, avoidance has become a go-to strategy to cope with your symptoms. This could be the way you avoid social situations, certain foods, intimacy with a partner, or traveling. And many people with IBS are hypervigilant about bathroom access at all times, which leads to further avoidance— and a lower quality of life.
Even though it may feel like avoiding situations beyond your comfort zone is the best way to manage your condition, researchers have found that how you choose to your IBS experiences often leads to the most anxiety and suffering.
Why anxiety worsens IBS
Unfortunately, scientists are still unsure how anxiety may cause or worsen your IBS symptoms.
One thought is that anxiety disorders and IBS are linked together by our ‘fight or flight’ response. Researchers have suggested that people with anxiety disorders and IBS tend to have stronger reactions to perceived sources of danger.
So, because you may be interpreting both environmental cues and sensations in your gut as harmful, this could lead to anxiety and IBS.
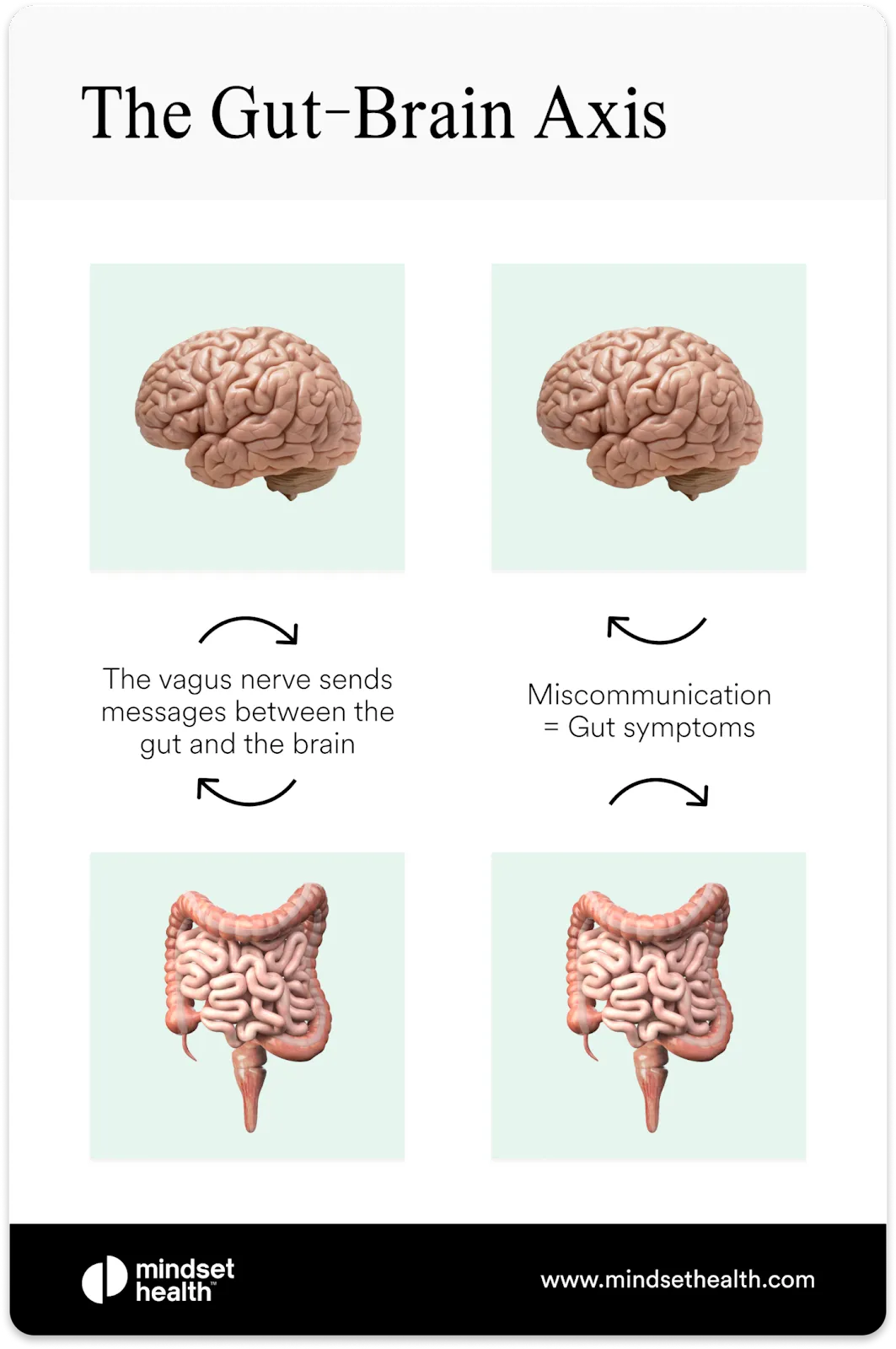
The gut-brain axis
The goings-on in your gut are closely connected to the thoughts circling around your mind thanks to the gut-brain axis, which could explain how anxiety influences your IBS and vice versa.
The gut-brain axis is the two-way communication channel between your bowel and brain. Messages travel back and forth along the vagus nerve—think of it as a superhighway of nerve fibers.
How your gut and brain influence each other can be explained in a few ways.
Firstly, microbes in your colon have been shown to affect your mental health and may even cause psychological illnesses such as anxiety disorder or depression. This could occur as a direct impact of the microbes themselves or how they may be causing inflammation in your GI tract. The way these microbes work in your gut also implies that your diet could directly impact your mental health.
Secondly, the biopsychosocial model also helps explain the link between anxiety and IBS.
This model was conceived in 1977, and it refers to the connection between our biological, psychological, and social interactions.
It explains how our social experiences, such as trauma, can lead to psychological and, in turn, biological effects. It also helps to explain how biological processes in IBS, such as distension of the bowel, can influence psychological distress and anxiety.
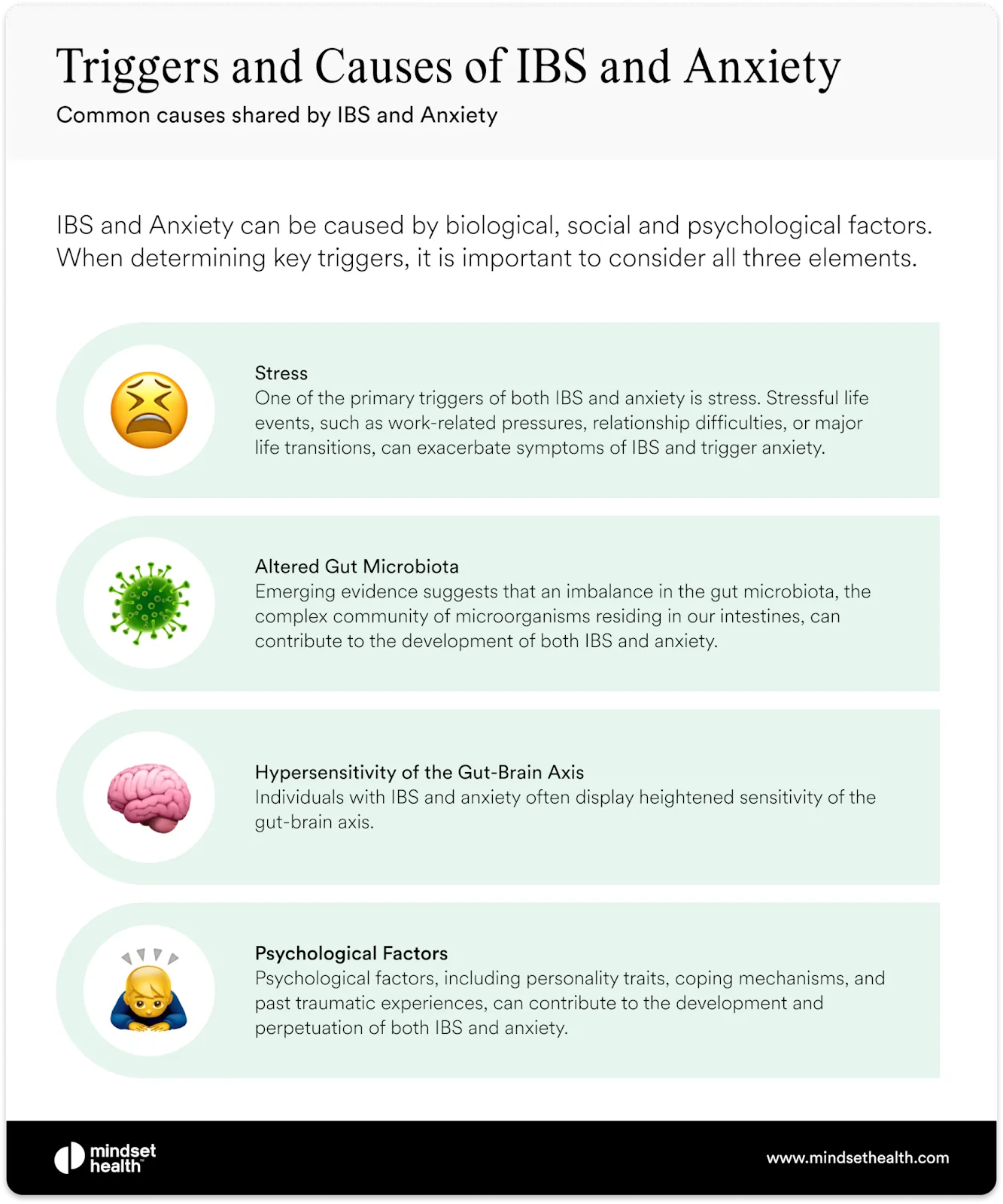
Triggers and Causes of IBS and Anxiety
IBS and anxiety share some common causes and triggers that are related to the gut-brain axis and biopsychosocial model as discussed above.
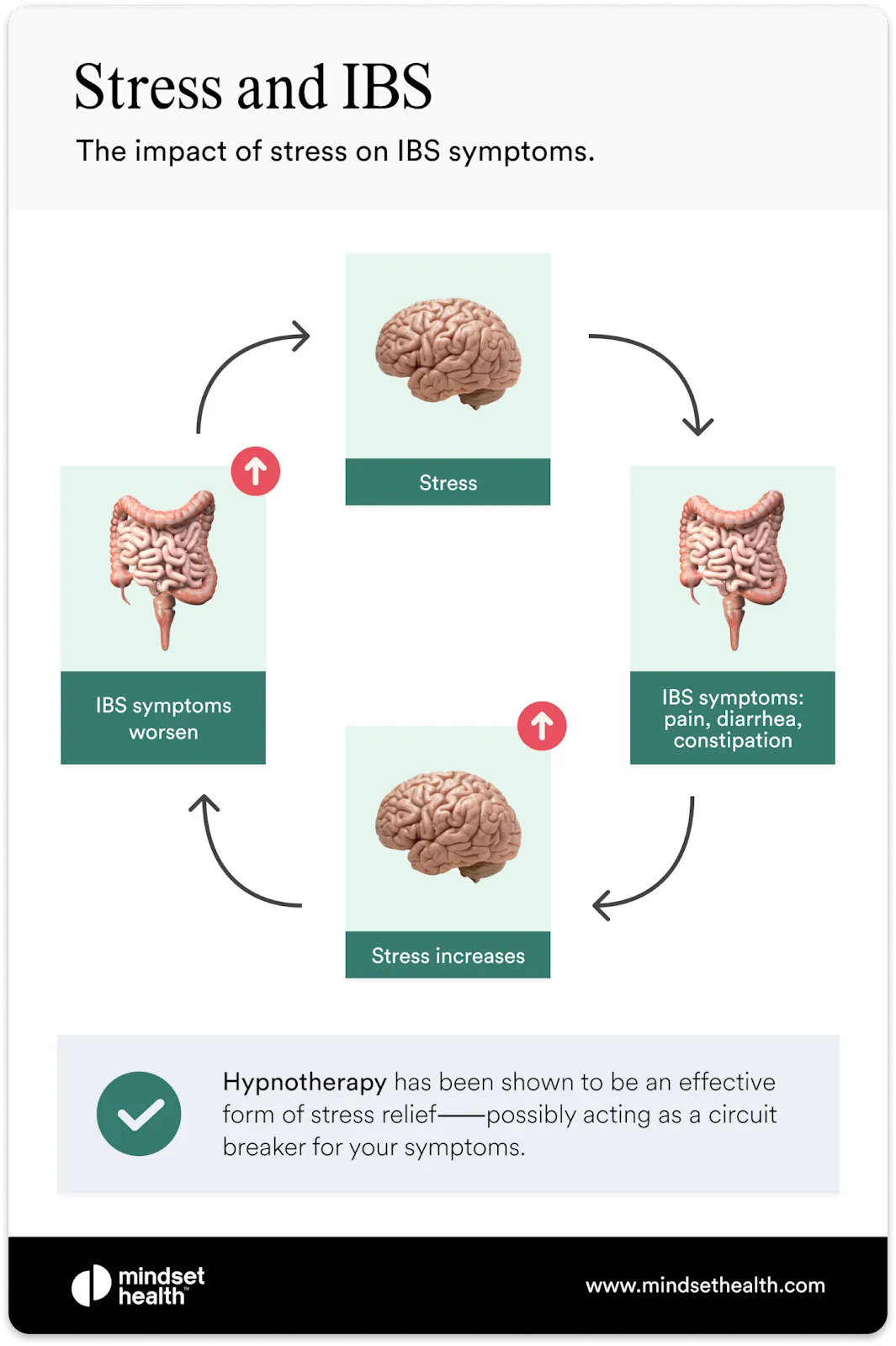
Stress
One of the primary triggers of both IBS and anxiety is stress. Stressful life events, such as work-related pressures, relationship difficulties, or major life transitions, can exacerbate symptoms of IBS and trigger anxiety. Stress activates the release of stress hormones like cortisol, which can impact gut motility, increase visceral sensitivity, and disrupt the delicate balance of the gut microbiota. These changes can lead to the onset or worsening of IBS symptoms and contribute to heightened anxiety levels.
Altered Gut Microbiota
Emerging evidence suggests that an imbalance in the gut microbiota, the complex community of microorganisms residing in our intestines, can contribute to the development of both IBS and anxiety. Disruptions in the composition and diversity of the gut microbiota, known as dysbiosis, have been linked to gastrointestinal symptoms and mood disorders. The gut microbiota produces neurotransmitters like serotonin, a key regulator of mood and intestinal function. Imbalances in serotonin levels, often observed in IBS and anxiety, can lead to alterations in gut motility, visceral hypersensitivity, and emotional well-being.
Hypersensitivity of the Gut-Brain Axis
Individuals with IBS and anxiety often display heightened sensitivity of the gut-brain axis. This means that normal gut sensations or stimuli that wouldn't typically elicit a response can trigger exaggerated and distressing symptoms. This hypersensitivity can manifest as visceral pain, increased awareness of bowel movements, or an amplified perception of gastrointestinal symptoms. The overactive communication between the gut and the brain amplifies discomfort, anxiety, and emotional distress, creating a vicious cycle where IBS symptoms exacerbate anxiety and vice versa.
Psychological Factors
Psychological factors, including personality traits, coping mechanisms, and past traumatic experiences, can contribute to the development and perpetuation of both IBS and anxiety. Individuals with a tendency towards perfectionism, high levels of neuroticism, or a history of childhood adversity may be more susceptible to developing both conditions. Moreover, coping strategies such as catastrophising, rumination, and avoidance behaviours can exacerbate symptoms and heighten anxiety levels, further entwining the two disorders.
Treatments for IBS and anxiety
While there’s no cure for IBS, it is a treatable condition that can be managed with hypnotherapy, cognitive behavioral therapy (CBT), mindfulness-based treatments, antidepressants, or elimination diets such as the low FODMAP diet.
Similarly, anxiety treatments also include CBT, hypnotherapy, and antidepressants.
As these treatments target your nervous system, they have the potential to treat both your IBS and anxiety.
Antidepressants
Tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed to help both your anxiety and IBS at the same time.
Tricyclic antidepressants: A 2015 study assessing several clinical trials found tricyclic antidepressants improved IBS symptoms overall compared to other antidepressants, and these could be a good first option to try.
Tricyclics, such as Desipramine (Norpramin) or Nortriptyline (Pamelor), may help with your abdominal pain and tend to work best for those with diarrhea-predominant IBS (IBS-D). Just keep in mind that there are known side effects with tricyclics like difficulty sleeping and urinating, dizziness, sexual challenges, and a dry mouth.
SSRIs: While there isn’t as much research supporting SSRIs as a treatment for IBS and anxiety, they have been effective for some people and have fewer side effects. If you have constipation-predominant IBS (IBS-C), speak with your doctor to see if these are a good option for you.
Hypnotherapy
Research has shown how hypnotherapy can improve your IBS symptoms—one study demonstrated how six weeks of hypnotherapy decreased IBS symptoms in 70% of people, making it equally as effective as the low FODMAP diet.
While there is research about how hypnotherapy can contribute to reducing mood and anxiety disorders, it’s generally not considered a treatment for mood disorders. Instead, it’s an aid to psychotherapy.
The hypnotic process involves reaching a state of deep relaxation. It allows you to probe more deeply into thoughts hidden from your conscious mind, teaching you coping skills through experiential learning.
CBT
CBT treatment is a type of talk therapy that treats both anxiety disorders and IBS by teaching you techniques and strategies to manage your condition and reduce stress.
Cognitive restructuring is one such technique that helps you end obsessive thought patterns related to your IBS. It helps grow your awareness of your distorted thinking, which could lead to reduced symptoms.
You’ll also be taught how to put other relaxation training strategies in place through CBT, such as diaphragmatic breathing. This technique activates your parasympathetic nervous system (the system responsible for controlling your body’s ability to relax), and it helps promote normal digestion and fewer gastrointestinal symptoms.
Low FODMAP diet for IBS
Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, better known as FODMAPs, are carbohydrates that may be making your IBS symptoms worse. Foods high in FODMAPs ferment more quickly in your oversensitive gut, leading to increased gas in your intestines, as well as digestive symptoms such as abdominal pain and bloating.
There’s evidence that switching to a low FODMAP diet can reduce your symptoms significantly. This in turn can benefit your anxiety as it can reduce your anxious, obsessive thoughts about your gut.
The Wrap Up
The connection between anxiety and IBS is complex, and both conditions can be incredibly frustrating and painful. The impact on your overall quality of life can be significant. Often
anxious feelings arise from unwanted sensations in your GI tract and from the fear of a flare-up. The gut-brain axis contributes to how your anxiety influences your IBS and vice versa. Treatments to help manage both conditions include hypnotherapy, CBT, antidepressants, and a low FODMAP diet.