The economic burden of IBS
IBS imposes a significant health-economic burden – not only on patients but across the healthcare system. In the United States, IBS-related costs exceed $21 billion each year, largely due to repeated investigations, pharmacotherapy, and fragmented management that fail to address the gut-brain mechanisms driving symptoms.¹
For patients with persistent or refractory presentations, these cycles contribute to escalating personal and system-level costs without corresponding functional gains.
AGA recognition of brain-gut therapies and digital access
The American Gastroenterological Association (AGA) has now formally recognized brain-gut behavior therapies (BGBT) – such as gut-directed hypnotherapy (GDH) – as evidence-based components of IBS management.²
Developed in collaboration with the Rome Foundation, the new AGA quality indicators emphasize that effective care must target the gut-brain axis directly through interventions like GDH or cognitive behavioral therapy.
Crucially, the AGA acknowledges that the main barriers preventing wider adoption of these therapies are cost, geography, and specialist availability.
Its inclusion of digital therapeutics as a scalable, validated alternative represents an important shift toward affordability and equity – recognizing that digital GDH can extend access to guideline-supported care without the cost burden of traditional delivery models.
Extending access to pediatric patients
Similarly, the European and North American Societies for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN and NASPGHAN) have updated their joint recommendations to include GDH for adolescents with functional abdominal pain disorders.³
This pediatric endorsement further highlights the need for accessible, lower-cost interventions that can be delivered beyond tertiary care settings – ensuring that adolescent IBS patients are not excluded from effective therapy due to financial or geographic limitations.
Evidence for cost reduction with digital GDH
Digital GDH programs such as Nerva operationalize these recommendations by delivering structured, evidence-based therapy through an accessible, app-based format.
At the 2024 Digestive Disease Week (DDW) conference, Monash University researchers led by Nerva's Dr. Simone Peters presented findings from a real-world analysis of more than 4,000 adults completing the Nerva program.
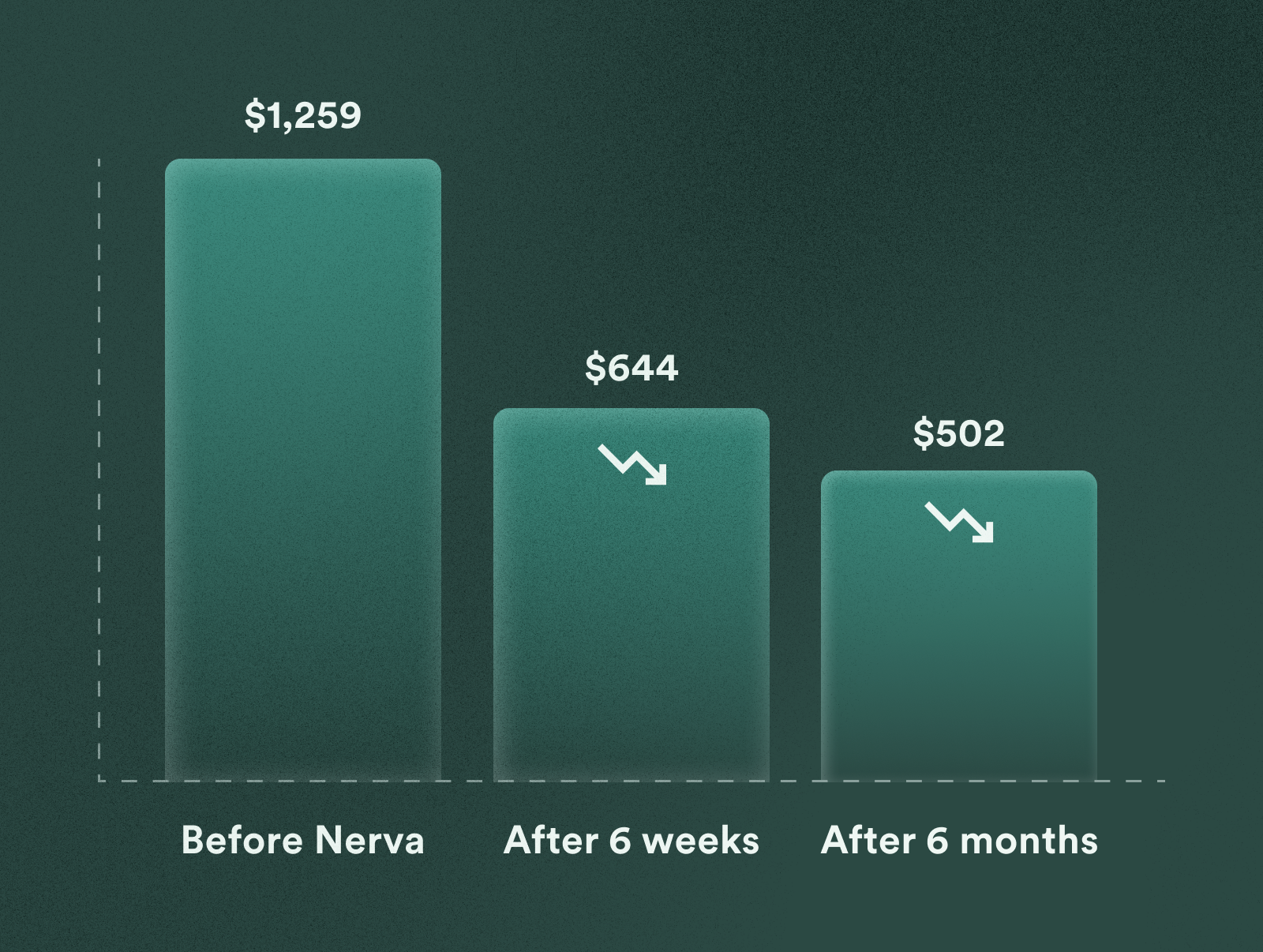
Patients’ self-reported IBS-related healthcare costs decreased from $1,259 in the six months prior to starting the program to $644 at completion and $502 at six-month follow-up – a reduction of more than 50%.⁴
Improvements in absenteeism, presenteeism, and work productivity further demonstrated the economic and functional value of accessible brain-gut therapies.
Reducing barriers through the Patient Assistance Program
To help address affordability, all patients referred through the online clinician form automatically receive a 25% referral adjustment, reducing the annual cost of Nerva to $186.75 AUD / $149.25 USD.
For patients experiencing financial hardship, Nerva’s Patient Assistance Program (PAP) offers an additional pathway to support – with coverage that can extend up to full access at no cost.
Clinicians simply refer as usual through the secure HIPAA-compliant online form, and Nerva contacts eligible patients directly to guide them through available assistance options. This ensures equitable access to evidence-based brain-gut therapy without creating extra administrative work for clinicians.

.jpeg)





